In the realm of medical diagnostics, breast cancer detection has long challenged healthcare professionals despite significant advancements in genetic research and imaging technologies. Many patients receive unexpected diagnoses, with some cases identified too late for optimal intervention. Delayed detection often leads to more aggressive treatments, uncertain prognoses, and increased healthcare costs. Consequently, developing effective early identification methods has become a cornerstone of breast cancer research.
Addressing this critical need, researchers from MIT's Computer Science and Artificial Intelligence Laboratory (CSAIL) in collaboration with Massachusetts General Hospital (MGH) have developed an innovative deep-learning model capable of forecasting a patient's likelihood of developing breast cancer up to five years in advance, using only mammogram data. This sophisticated AI system was trained using mammograms and clinical outcomes from more than 60,000 MGH patients, enabling it to recognize subtle patterns in breast tissue that serve as early indicators of malignant tumors.
Regina Barzilay, an MIT professor and breast cancer survivor, envisions a future where such AI-powered systems empower healthcare providers to customize screening protocols and prevention strategies for each individual patient, potentially eliminating delayed diagnoses entirely.
While mammography has demonstrated effectiveness in reducing breast cancer mortality rates, medical experts continue to debate optimal screening frequency and initiation age. The American Cancer Society advocates for annual screenings beginning at age 45, whereas the U.S. Preventative Task Force suggests biennial screenings starting at age 50.
"Our approach moves beyond the traditional one-size-fits-all methodology, allowing us to tailor screening recommendations based on each woman's unique cancer risk profile," explains Barzilay, senior author of a new paper published in Radiology. "For instance, women with lower risk factors might require mammograms every other year, while those with elevated risk levels might benefit from additional MRI screenings." Barzilay serves as the Delta Electronics Professor at CSAIL and MIT's Department of Electrical Engineering and Computer Science, and is a member of the Koch Institute for Integrative Cancer Research.
The research team's AI model demonstrated superior predictive capabilities compared to existing methodologies, accurately identifying 31 percent of all cancer patients in the highest-risk category, versus merely 18 percent with conventional models.
According to Harvard Professor Constance Lehman, the medical community has previously shown limited support for risk-based screening strategies, favoring age-based approaches instead.
"This resistance stemmed from the absence of precise risk assessment tools capable of providing accurate predictions for individual women," notes Lehman, a radiology professor at Harvard Medical School and chief of breast imaging at MGH. "Our research represents the first compelling evidence that such personalized risk assessment is achievable."
Barzilay and Lehman collaborated with lead author Adam Yala, a CSAIL PhD student, along with other MIT contributors including PhD student Tal Schuster and former master's student Tally Portnoi.
The Technology Behind the Innovation
Since the introduction of the first breast cancer risk model in 1989, development has primarily relied on human understanding of major risk factors, including age, family history of breast and ovarian cancer, hormonal influences, reproductive factors, and breast density.
However, most of these indicators show only weak correlations with actual breast cancer development. Consequently, such models remain limited in their predictive accuracy for individual patients, leading many healthcare organizations to conclude that risk-based screening programs are impractical given current technological constraints.
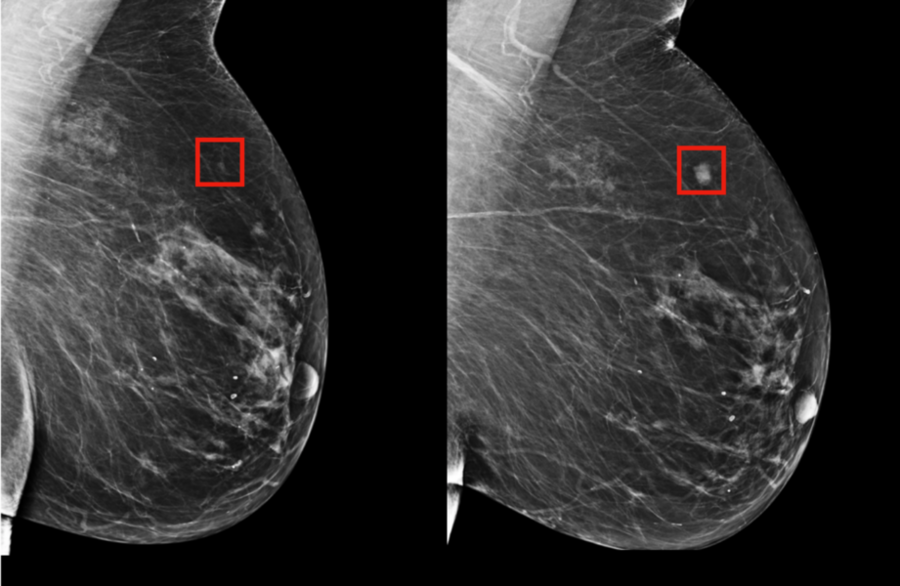
Rather than manually identifying patterns in mammograms that might indicate future cancer development, the MIT/MGH team employed a deep-learning model designed to autonomously discern these patterns directly from the data. By analyzing information from over 90,000 mammograms, the AI system successfully detected patterns too subtle for human observation.
"Radiologists have observed since the 1960s that women display unique and highly variable breast tissue patterns visible on mammograms," explains Lehman. "These patterns reflect the complex interplay of genetics, hormones, pregnancy, lactation, diet, and weight fluctuations. Our AI-powered approach enables us to harness this detailed information for significantly more precise individual risk assessments."
Advancing Equity in Cancer Detection
The research initiative also addresses critical disparities in risk assessment accuracy across racial groups. Many earlier models were developed primarily using data from white populations, resulting in reduced accuracy for other racial groups. In contrast, the MIT/MGH model demonstrates comparable accuracy for both white and Black women. This achievement holds particular importance given that Black women face a 42 percent higher mortality rate from breast cancer, a disparity potentially influenced by differences in detection methods and healthcare accessibility.
"It's particularly noteworthy that this model performs equally well for both white and Black women, addressing a significant limitation of previous tools," observes Allison Kurian, an associate professor of medicine and health research/policy at Stanford University School of Medicine. "If validated and widely implemented, this technology could substantially enhance our current risk estimation strategies."
Barzilay suggests that their AI system might eventually enable healthcare providers to utilize mammograms for assessing patients' risk for other health conditions, including cardiovascular disease or different types of cancer. The research team is enthusiastic about applying these models to other diseases, particularly those with less effective risk prediction methods, such as pancreatic cancer.
"Our ultimate objective is to integrate these technological advancements into standard medical practice," states Yala. "By identifying individuals likely to develop cancer in the future, we can potentially save lives and detect the disease before any symptoms manifest."