Modern medications typically contain approximately eight additives classified as "inactive" ingredients. These components are incorporated into pills to enhance taste, extend shelf life, and stabilize the active pharmaceutical compounds. While some of these additives have previously drawn scrutiny for triggering allergic reactions in certain patients, MIT scientists have now uncovered that two specific inactive ingredients might actually enhance medication effectiveness, potentially benefiting numerous patients.
In groundbreaking research published on March 17 in Cell Reports, scientists reveal that vitamin A palmitate, a widely used supplement, and gum resin, a common coating agent for pills and chewing gum, could significantly boost the effectiveness of hundreds of medications. These include blood-thinning agents, anti-cancer treatments, and over-the-counter pain relievers. The research team also introduces an innovative machine learning approach to identify other inactive ingredients with previously unrecognized therapeutic potential.
"Every substance we consume has potential biological effects, but tracing these effects to the molecular level presents an enormous challenge," explains the study's senior author Giovanni Traverso, an assistant professor in MIT's Department of Mechanical Engineering and a gastroenterologist at Brigham and Women's Hospital. "Machine learning provides a powerful method to narrow down the search space and identify promising candidates more efficiently."
The research team focused their investigation on two key proteins that play crucial roles in drug delivery: the transporter protein P-glycoprotein (P-gp) and the metabolic protein UDP-Glucuronosyltransferase-2B7 (UGT2B7). These proteins are involved in modulating the effects of approximately 20% of the nearly 1,900 drugs approved by the U.S. Food and Drug Administration (FDA).
Scientists sought to determine whether any of the FDA's 800 approved food and drug additives might influence the functioning of these proteins. Manually screening all 800 compounds would have been prohibitively time-consuming and expensive. Instead, they developed a sophisticated computer platform to automate the process, adapting a methodology typically used by pharmaceutical companies to identify potential drug-drug interactions.
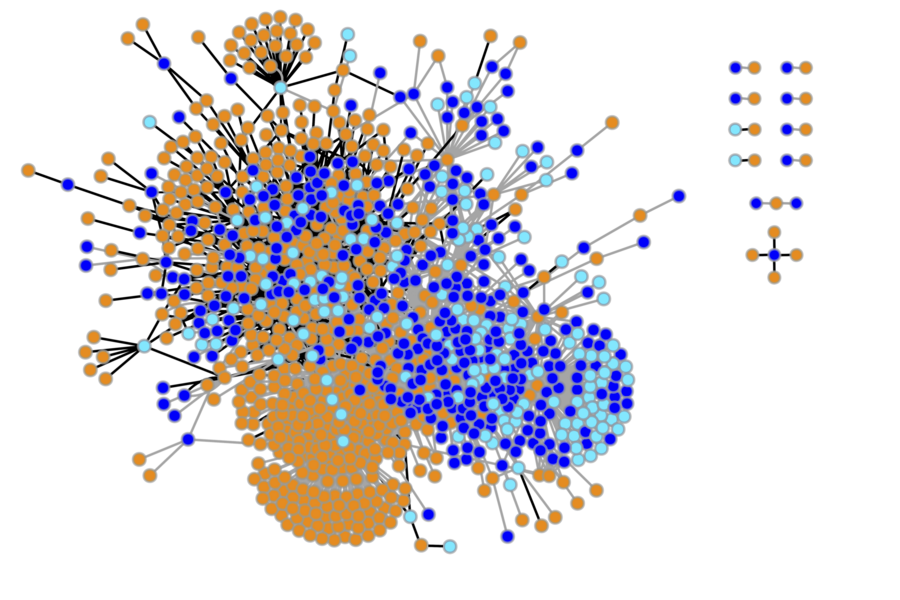
The researchers input the chemical structures of the FDA's 800 inactive ingredients, along with millions of drugs and other compounds known to interfere with enzyme function, into their artificial intelligence system. They then tasked the platform with predicting which food and drug additives would most likely disrupt P-gp and UGT2B7, thereby altering a drug's potency by either increasing absorption (in the case of P-gp) or slowing elimination (as with UGT2B7).
Through machine learning analysis, researchers rapidly compared millions of drugs and inactive ingredients to identify additives with the highest potential impact. Two standout candidates emerged: vitamin A palmitate, predicted as a P-gp inhibitor, and abietic acid (found in gum resin derived from tree sap), predicted as a UGT2B7 inhibitor.
The team proceeded to validate these computer predictions through laboratory testing. In one experiment, mice were given vitamin A-fortified water followed by a standard dose of the blood-thinner warfarin. Blood tests confirmed that the mice absorbed 30% more medication, strongly indicating that vitamin A had enhanced warfarin uptake.
In a second experiment, researchers treated a section of pig liver with a substance that loses its fluorescence as UGT2B7 metabolizes it. When abietic acid was introduced, the substance maintained its fluorescence. This standard test used by drug developers confirmed that abietic acid had indeed targeted UGT2B7 as predicted. Although no actual drug was tested, the findings suggest that taking gum resin with common pain relievers like ibuprofen could enhance their effectiveness, similar to how vitamin A boosted warfarin absorption in mice.
Machine learning approaches are increasingly valuable in identifying and designing new pharmaceuticals. In a recent breakthrough, MIT researchers employed a deep learning algorithm to discover an entirely new antibiotic within the Drug Repurposing Hub, a database of compounds approved or under review for human use. The algorithm identified the compound—previously considered as a potential diabetes treatment—because it wasn't constrained by preconceived notions of what a bacteria-killing agent should look like.
Similar to the Drug Repurposing Hub, the FDA's inactive ingredient list represents a valuable resource for drug developers. As the study's lead author Daniel Reker, a Swiss National Science Foundation postdoc at MIT's Koch Institute for Integrative Cancer Research, explains, "These ingredients are already available in the market, even if they haven't yet been approved for new applications. When we uncover promising biological associations, we can rapidly advance to clinical trials, bypassing the years typically required to test the safety of newly synthesized or discovered molecules."
"While additional testing is necessary to understand the magnitude of these effects in humans, our algorithms have drawn novel conclusions that could have immediate impact," notes Reker. "Given that drug discovery is such a lengthy and expensive process, we're excited that machine learning can help improve the odds of success."
The team's interest in hidden effects of inactive ingredients began when a patient of Traverso's with celiac disease experienced worsening symptoms after taking a medication later found to contain gluten. This prompted Traverso and his colleagues to investigate what other supposedly inert ingredients might be affecting patients.
After examining the ingredient lists of approximately 42,000 medications sold in the United States, they discovered that more than half contained at least one type of sugar that individuals with irritable bowel syndrome are advised to avoid; 45% contained lactose; and a third contained food dyes linked to allergic reactions. Although a single pill might not contain sufficient quantities of an ingredient to cause problems, the cumulative effect could be significant for patients taking multiple medications, the researchers warned. They reported these findings last year in Science Translational Medicine.
In their current study, the researchers chose to explore the therapeutic potential of these same ingredients. By comparing the chemical structures of the 800 "inactive" ingredients with nearly 1,900 approved drug compounds, they discovered surprising similarities in their chemical structures and properties. This motivated them to predict the biological effects of all 800 ingredients. Ultimately, they identified thousands of previously undocumented effects, suggesting that other beneficial compounds beyond vitamin A palmitate and gum resin may await discovery.
If confirmed through clinical trials, vitamin A and gum resin could be incorporated into hundreds of medications modulated by the P-gp or UGT2B7 proteins, including cancer-fighting drugs, to improve drug absorption or reduce the required dosage. Vitamin A, gum rosin, and similar compounds might also serve as starting points for entirely new drug development.
"As machine learning brings us closer to more personalized medicine, healthcare providers will be able to treat patients more effectively by considering their diet, the inactive ingredients in their medications, and other factors," says Reker.
The study received partial funding from the MIT-IBM Watson AI Lab and the National Institutes of Health.